由于随机对照研究数据有限,目前尚不明确补充维生素D能否减少癌症或心血管疾病的发生风险。
正值第十个全球双十一购物狂欢节之际,美国麻省医学会《新英格兰医学杂志》于美国东部时间2018年11月10日在线连发两篇
哈佛大学医学院、哈佛大学陈曾熙公共卫生学院、布列根医院和波士顿妇女医院
的随机对照研究(VITAL)报告,向维生素D和海洋鱼油保健品消费市场泼了一些冷水。
VITAL
: Vitamin D and Omega-3 Trial (NCT01169259)
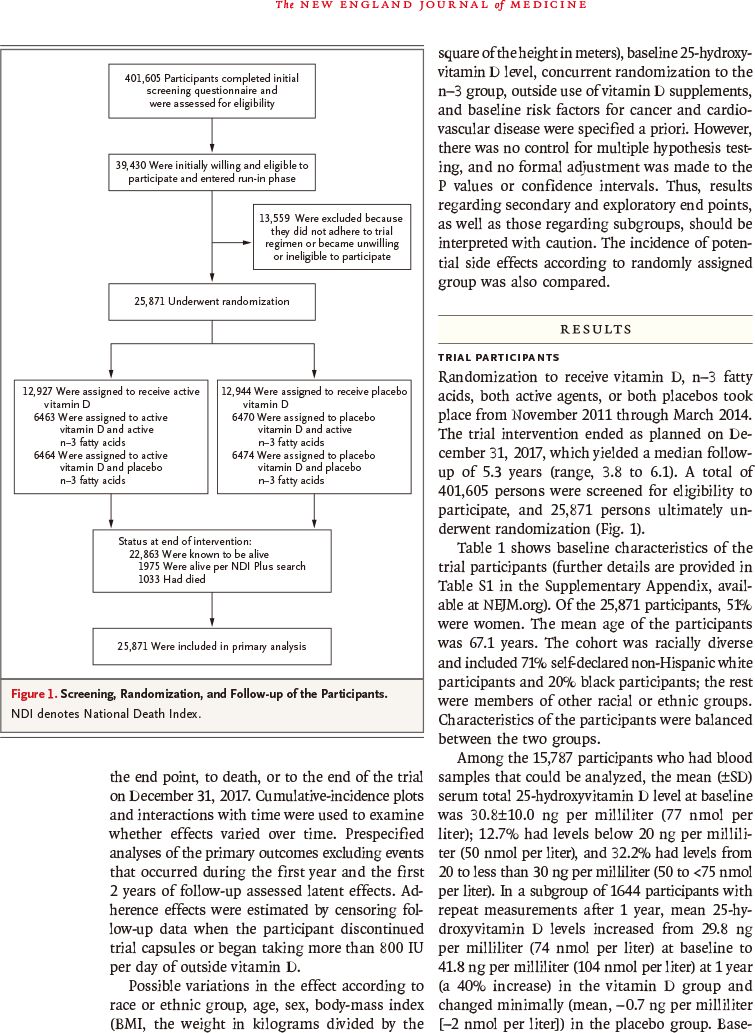
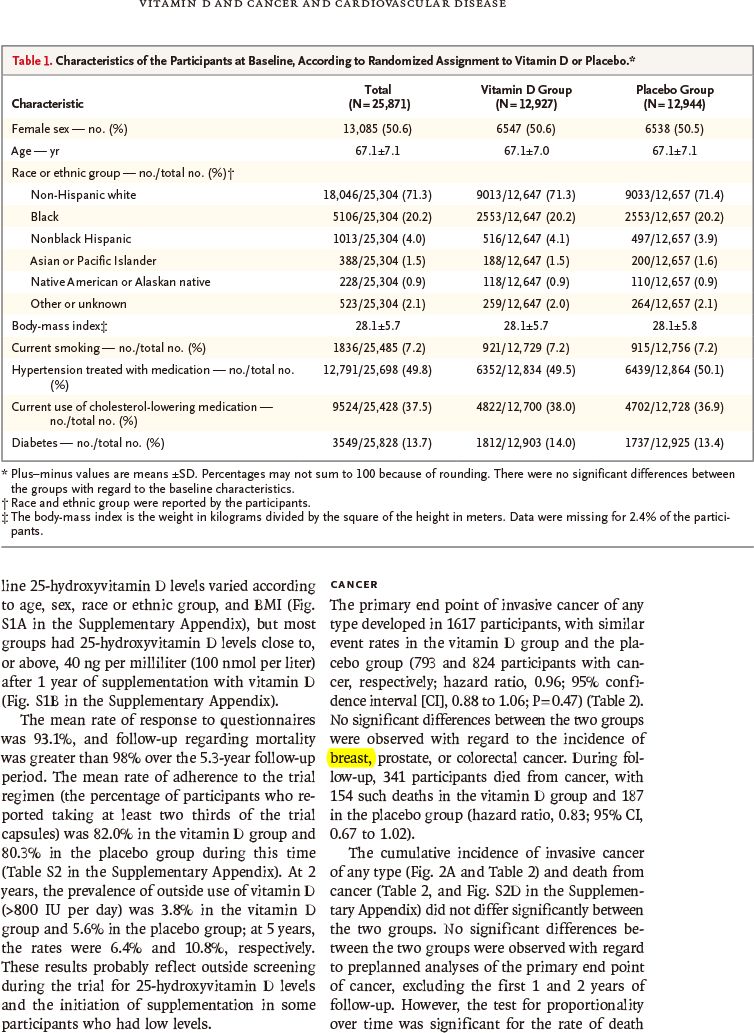
该全国随机双盲安慰剂对照前瞻干预研究于2011年11月~2014年3月从美国招募
1万2786位年龄≥50岁男性
和
1万3085位年龄≥55岁女性
志愿者,按1∶1随机分组,每天口服
2000国际单位维生素D3(胆钙化醇)、1克海洋鱼油n-3(又称ω-3)脂肪酸或安慰剂
,以观察维生素D3、n-3脂肪酸对癌症和心血管疾病发生风险的一级预防作用。该研究由美国国家卫生研究院等提供资助。为了减少偏倚,该研究采用了2×2因子设计:
-
6463位志愿者:维生素D3+n-3脂肪酸
-
6464位志愿者:维生素D3+安慰剂
-
6470位志愿者:安慰剂+n-3脂肪酸
-
6474位志愿者:安慰剂+安慰剂
主要观察终点为任何类型浸润癌和重要心血管事件(心肌梗塞、中风、心血管所致死亡),次要观察终点包括地区相关癌、癌症所致死亡、其他心血管事件以及安全性。本文报告了维生素D与安慰剂的比较结果。
结果发现,补充维生素D与任何主要观察终点的发生风险减少无显著相关性。
随访时间3.8~6.1年(中位5.3年)
期间,维生素D组与安慰剂组相比:
-
被诊断出浸润癌:793例比824例(风险比:0.96;95%置信区间:0.88~1.06,P=0.47)
-
重要心血管事件:396例比409例(风险比:0.97,95%置信区间:0.85~1.12,P=0.69)
-
被诊断出
乳腺癌
:124例比122例(风险比:1.02,95%置信区间:0.79~1.31)
-
被诊断前列腺癌:192例比219例(风险比:0.88,95%置信区间:0.72~1.07)
-
被诊断结直肠癌:51例比47例(风险比:1.09,95%置信区间:0.73~1.62)
-
心肌梗死:169例比176例(风险比:0.96,95%置信区间:0.78~1.19)
-
中风卒中:141例比149例(风险比:0.95,95%置信区间:0.76~1.20)
-
冠状动脉血管重建:536例比558例(风险比:0.96,95%置信区间:0.86~1.08)
-
心血管病所致死亡:152例比138例(风险比:1.11,95%置信区间:0.88~1.40)
-
任何癌症所致死亡:154例比187例(风险比:0.83,95%置信区间:0.67~1.02)
-
任何原因所致死亡:485例比493例(风险比:0.99,95%置信区间:0.87~1.12)
此外,未见高钙血症或其他不良事件风险增加。
因此,该研究结果表明,补充维生素D与安慰剂相比,不会引起浸润癌或重要心血管事件发生率减少。
相关阅读
N Engl J Med. 2018 Nov 10. [Epub ahead of print]
Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease.
JoAnn E. Manson, Nancy R. Cook, I-Min Lee, William Christen, Shari S. Bassuk, Samia Mora, Heike Gibson, David Gordon, Trisha Copeland, Denise D'Agostino, Georgina Friedenberg, Claire Ridge, Vadim Bubes, Edward L. Giovannucci, Walter C. Willett, Julie E. Buring; VITAL Research Group.
Brigham and Women's Hospital, Harvard Medical School, Harvard T.H. Chan School of Public Health, Boston.
BACKGROUND
: It is unclear whether supplementation with vitamin D reduces the risk of cancer or cardiovascular disease, and data from randomized trials are limited.
METHODS
: We conducted a nationwide, randomized, placebo-controlled trial, with a two-by-two factorial design, of vitamin D3 (cholecalciferol) at a dose of 2000 IU per day and marine n-3 (also called omega-3) fatty acids at a dose of 1 g per day for the prevention of cancer and cardiovascular disease among men 50 years of age or older and women 55 years of age or older in the United States. Primary end points were invasive cancer of any type and major cardiovascular events (a composite of myocardial infarction, stroke, or death from cardiovascular causes). Secondary end points included site-specific cancers, death from cancer, and additional cardiovascular events. This article reports the results of the comparison of vitamin D with placebo.
RESULTS
: A total of 25,871 participants, including 5106 black participants, underwent randomization. Supplementation with vitamin D was not associated with a lower risk of either of the primary end points. During a median follow-up of 5.3 years, cancer was diagnosed in 1617 participants (793 in the vitamin D group and 824 in the placebo group; hazard ratio, 0.96; 95% confidence interval [CI], 0.88 to 1.06; P=0.47). A major cardiovascular event occurred in 805 participants (396 in the vitamin D group and 409 in the placebo group; hazard ratio, 0.97; 95% CI, 0.85 to 1.12; P=0.69). In the analyses of secondary end points, the hazard ratios were as follows: for death from cancer (341 deaths), 0.83 (95% CI, 0.67 to 1.02); for breast cancer, 1.02 (95% CI, 0.79 to 1.31); for prostate cancer, 0.88 (95% CI, 0.72 to 1.07); for colorectal cancer, 1.09 (95% CI, 0.73 to 1.62); for the expanded composite end point of major cardiovascular events plus coronary revascularization, 0.96 (95% CI, 0.86 to 1.08); for myocardial infarction, 0.96 (95% CI, 0.78 to 1.19); for stroke, 0.95 (95% CI, 0.76 to 1.20); and for death from cardiovascular causes, 1.11 (95% CI, 0.88 to 1.40). In the analysis of death from any cause (978 deaths), the hazard ratio was 0.99 (95% CI, 0.87 to 1.12). No excess risks of hypercalcemia or other adverse events were identified.
CONCLUSIONS
: Supplementation with vitamin D did not result in a lower incidence of invasive cancer or cardiovascular events than placebo.
Funded by
the National Institutes of Health
VITAL ClinicalTrials.gov number
: NCT01169259
DOI
: 10.1056/NEJMoa1809944





以下广告内容与本微信公众号无关





