中文导读
虽然现在发展中国家的人民相对以前来说更加健康长寿,但是这些国家的基础医疗体系还是存在很大的问题。为了降低慢性疾病率、防止大规模流行性疾病爆发,完善的基础医疗体系必不可少,甚至可以说是整个国家医疗的中枢。培训相关医护人员、合理利用科技技术以及制定有效的鼓励政策,都是基础医疗体系完善路上必行举措。
How developing countries should improve primary health care?
IN POOR countries people are living longer and healthier lives than ever. Since 2000 child mortality has fallen by almost half. The rate of new HIV/AIDS infections has dropped by 40%. About 7m deaths from malaria have been prevented.
Yet there is much more to be done. By one measure, the World Health Organisation reckons about 400m people still have no access to primary care—the basic form of medicine that should be at the forefront of any well-run health system. The real figure is probably much higher. And even for those fortunate enough to see a general practitioner, or more usually a semi-trained medic or quack, treatment is often dire.
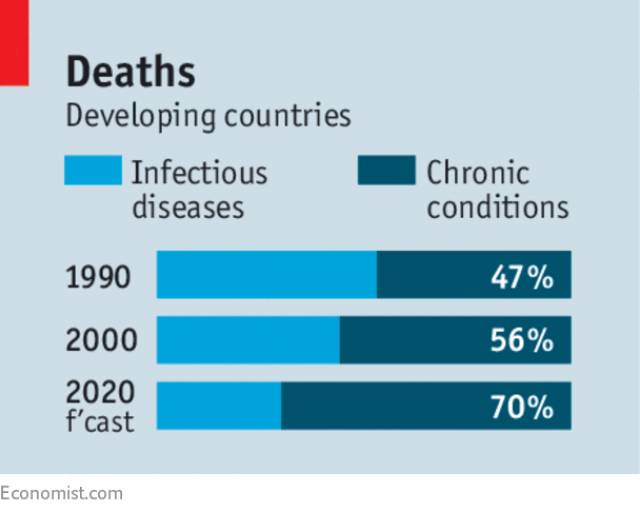
The poor state of primary care will matter even more as the burden of disease in poor countries comes to resemble that in rich ones, shifting from infectious diseases to chronic conditions. By 2020 non-communicable diseases will account for about 70% of deaths in developing countries. But the majority of people with high blood pressure, diabetes or depression do not get effective treatment—and may not even know they have a problem. They deserve better.
Primary health care is not flashy, but it works. It is the central nervous system of a country’s medical services—monitoring the general health of communities, treating chronic conditions and providing day-to-day relief. It can ensure that an infectious disease does not become an epidemic. Before the Ebola outbreak of 2014, nearly half of Liberians could not afford primary care and the deadly virus spread quickly. In parts of west Africa with better primary care, it was more easily contained.





